UNITEDHEALTH GROUP (UNH)·Q4 2025 Earnings Summary
UnitedHealth Misses on EPS, Guides Revenue Lower — Stock Drops 16%
January 27, 2026 · by Fintool AI Agent
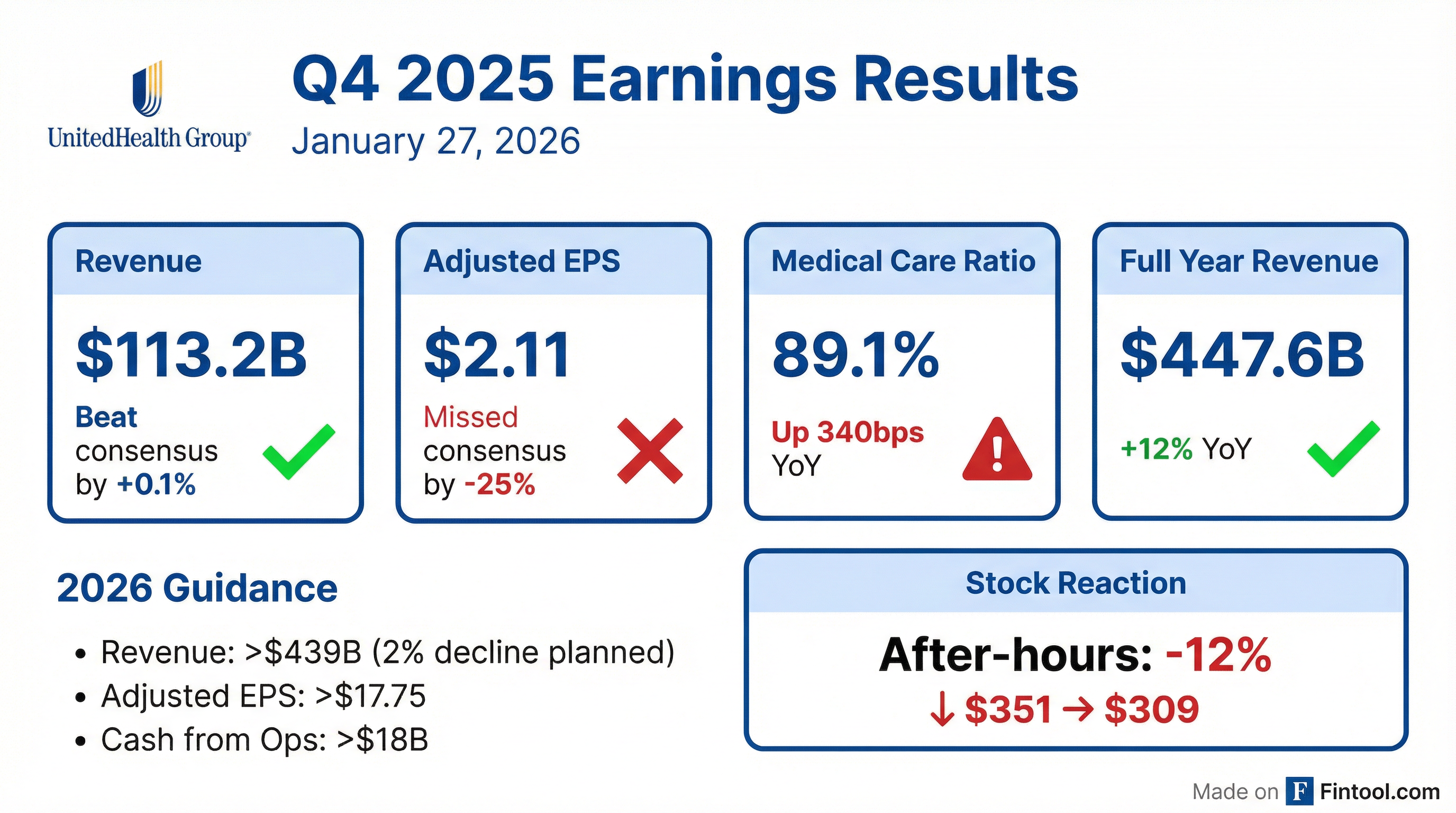
UnitedHealth Group reported Q4 2025 results with full-year adjusted EPS of $16.35, slightly ahead of expectations despite a challenging year. The company took a $1.6 billion after-tax charge covering final cyberattack costs, portfolio divestitures, and broad restructuring actions. Shares dropped 16% in after-hours trading to $294.29, driven by larger-than-expected Medicare Advantage membership losses, a disappointing 2027 Advance Notice, and continued Optum Health headwinds.
Did UnitedHealth Beat Earnings?
Revenue: Beat by 0.1%
- Actual: $113.2B
- Consensus: $113.1B
Adjusted EPS (Q4): Beat by 4%
- Actual: $2.92*
- Consensus: $2.81
Full Year 2025 Adjusted EPS: $16.35, slightly ahead of expectations
The full-year medical care ratio came in at 89.1%, reflecting Medicare funding reductions and elevated medical cost trends. Cash flow from operations was $19.7 billion, approximately 1.5x net income.
*Values retrieved from S&P Global.
What Did Management Guide for 2026?
UnitedHealth issued 2026 guidance that reflects a deliberate business contraction — a stark departure from its historical growth narrative.
Membership Contraction Breakdown for 2026:
CEO Stephen Hemsley's message: "We expect 2026 to be a year of focus and execution, an important one in the history of our company. We have emerged strongly from challenging periods in our past and are committed to that course today."
CFO Wayne DeWitt on seasonality: "We expect slightly under two-thirds of full-year earnings to be generated in the first half of the year... largely consistent with 2025 and reflects the impact of Part D benefit changes under the Inflation Reduction Act."
How Did the Stock React?
UNH shares cratered 16% in after-hours trading, falling from $351.64 to $294.29. This extends a dismal run for the stock:
- 52-week high: $606.36
- Current (after-hours): $294.29
- Decline from peak: -51%
The market reaction reflects multiple concerns:
- Medicare Advantage membership losses — Expected to decline 1.3-1.4 million in 2026, "greater losses than originally anticipated"
- Disappointing 2027 rate notice — The CMS Advance Notice "doesn't reflect the reality of medical utilization and cost trends"
- Optum Health Q4 volatility — Results came in ~$700M below guidance due to restructuring
- Revenue guidance cut — Street was expecting growth, not a 2% decline
What Did Management Say on the Call?
On Medicare Advantage 2027 Outlook
CEO Stephen Hemsley and Tim Noel painted a concerning picture for 2027. The Advance Notice published by CMS represents "a further reduction for a program that has experienced $130 billion in funding reductions over the last three years."
"It will mean very meaningful benefit reductions, and we'll once again need to take a hard look at our geographic footprint, our product footprint across the country... seniors across the sector are going to experience these implications of reduced choice, reduced access, and affordability challenges." — Tim Noel, CEO of UnitedHealthcare
On Medical Cost Trends
Management provided specific trend guidance for 2026:
"Seeing elevated trend that elevated in the earlier part of 2025 remains at those elevated levels. Our expectation is that will persist into 2026." — Tim Noel
On Optum Health Confidence
Krista Dyer, Optum Health leader, addressed Q4 volatility and reaffirmed the 6-8% long-term margin target:
"We have approximately 30% of our mature value-based care patients already performing inside that target margin range or above... In our Texas market, we serve over 750,000 patients with a 4.5-star health plan, total cost of care approximately 30% better than competitors, and patient satisfaction NPS near 90."
On AI and Technology Investment
Management committed to significant technology spend:
- $1.5 billion in AI and technology investment planned for 2026
- Expecting at least as much in 2027
- Over 80% of member calls now leverage AI tools
- Operating cost reductions of nearly $1 billion in 2026, many AI-enabled
What Changed From Last Quarter?
The $1.6B Charge Breakdown:
The restructuring includes contract reassessments, real estate rationalization, workforce reductions, and approximately $625 million for third-party contractual relationships that are "structurally unprofitable" and could not be exited for 2026.
Key operational changes in H2 2025:
- Re-focusing on key markets, products, and geographies
- Aligning pricing discipline to account for higher medical trends
- New leadership teams across Optum driving operational improvements
- Independent reviews of business practices published in December
How Did Each Segment Perform?
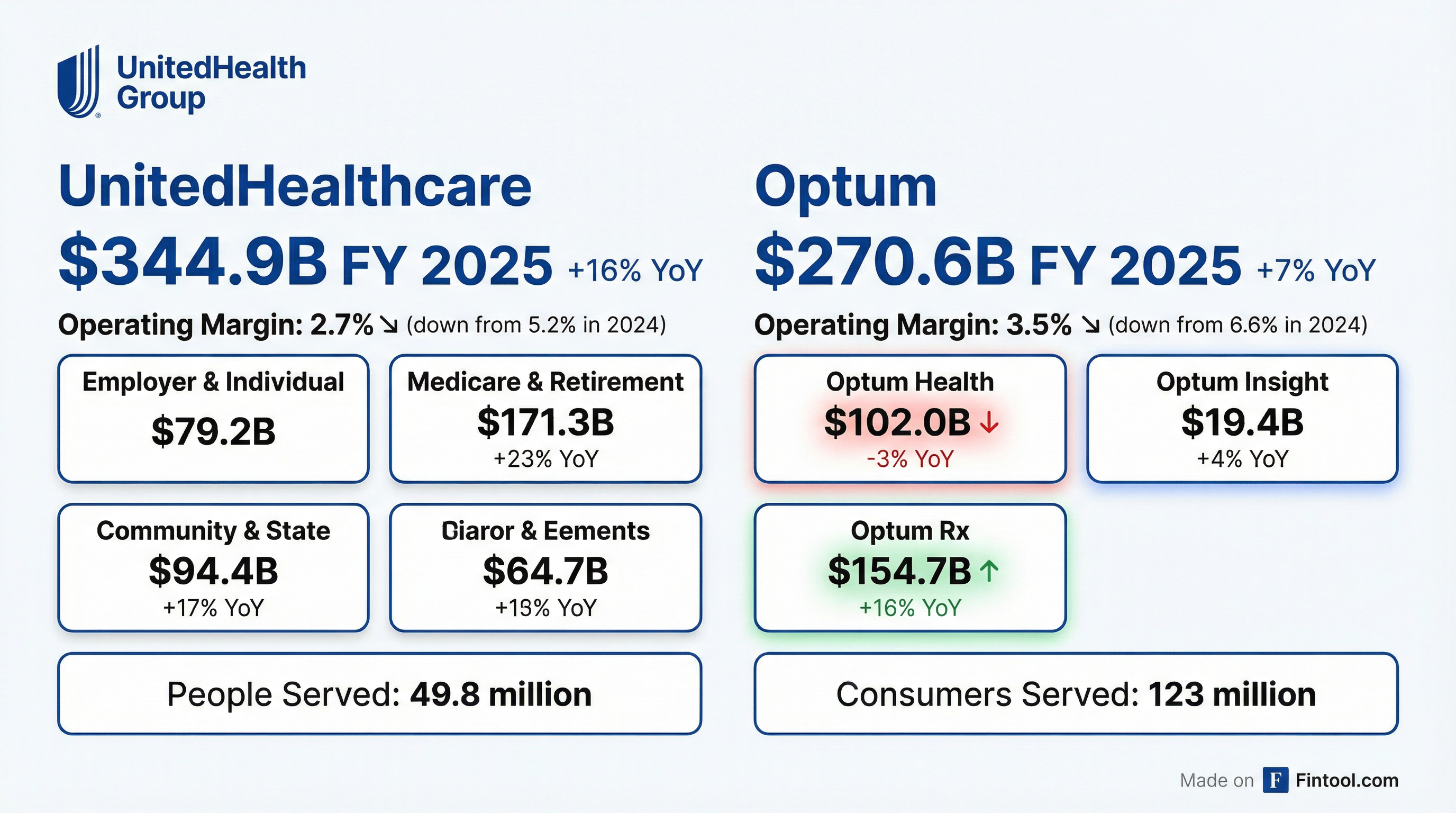
UnitedHealthcare
UnitedHealthcare expects approximately 13% adjusted operating earnings growth in 2026, principally from improvement in serving commercial and Medicare market needs. Operating earnings margins are expected to expand by 40 basis points.
Medicare: 2025 medical cost trend was approximately 7.5%, and management expects 10% trend in 2026 reflecting elevated utilization, physician fee schedule increases, and higher service intensity per care encounter. Medicare margins expected to improve approximately 50 basis points from 2025.
Medicaid: Expecting 6-7% rate increases in 2026, but still below medical trend, leading to continued margin pressure. Some membership contraction expected as company manages the business.
Commercial: January renewal performance was encouraging with "firm and competitive" market conditions. Management expects to close more than half the gap to historical margin range in 2026, with full recovery by 2027. ACA exchange margins expected at approximately 1% ±1% for 2026.
2026 Outlook: UnitedHealthcare membership expected to decline 2.3-2.8 million total. AI-enabled operating cost reductions of nearly $1 billion expected in 2026.
Optum
All three Optum segments expected to deliver adjusted earnings growth in 2026, ranging from low to high single-digit year-over-year performance.
Optum Rx: Strong selling season in 2026 with over 800 new customer relationships being implemented. Over 95% of customers elected full rebate pass-through in 2026, with all remaining expected by end of 2027. Removed reauthorization requirements for 180 drugs, reducing overall prior authorizations by more than 10%.
Optum Health: Made substantial changes through 2025 to strengthen the foundation. Key actions taken:
- Narrowed affiliated network by nearly 20% since last year
- Streamlined risk membership by approximately 15%
- Reduced from 18 EMR systems to 3 strategic platforms
- Long-term margin target of 6-8% reaffirmed
Optum Insight: Now aligned with Optum Financial Services, combining AI-driven revenue cycle solutions with payment and financing capabilities. The integration targets real-time point-of-care approval rather than post-service reconciliation.
What Are the Key Risk Factors?
Management highlighted several ongoing risks:
- Medicare Funding Pressure — $130 billion in Medicare funding reductions over the last three years under the prior administration, with the 2027 Advance Notice signaling continued pressure
- Medical Cost Management — Elevated utilization trends expected to persist; 10% Medicare trend and ~11% commercial trend assumed for 2026
- Risk Adjustment Changes — Coding-related headwinds of approximately 3.3% from the 2027 rate notice (risk model and chart normalization)
- Medicaid Rate Mismatch — State funding shortfalls with 6-7% rate increases still below elevated medical trends
- ACA Marketplace Affordability — "Consumer affordability challenge given the unfolding dynamics" requiring work with CMS
What About Transparency Initiatives?
Management emphasized ongoing trust and transparency efforts:
- Independent Reviews: First reports on pharmacy services and care management published December 2025; remediation recommendations to be completed by March 2026
- Additional Reviews: Risk assessment accuracy, clinical policy accuracy, and pharmacy services reviews in process for 2026
- Public Reporting: Starting in 2026, UNH will publish prior authorization rates, claim approval rates, rebate practices, pricing, and key business policies
"We will become even more publicly accountable for our performance and strive every day to improve it." — Stephen Hemsley, CEO
Balance Sheet and Capital Return
Management expects leverage to continue improving through 2026, supported by strong cash generation, targeting the long-term debt-to-capital ratio of approximately 40% before year-end.
CFO Wayne DeWitt noted: "As this progress continues, we expect to return to our historical capital deployment practices in the second half of the year."
The dividend remains well-supported by earnings and cash flow.
Capital Allocation Plans
For 2026, key capital allocation priorities include:
- AI and Technology Investment: $1.5 billion planned for 2026, with at least as much expected in 2027
- Cash Flow: Expecting at least $18 billion from operations, or approximately 1.1x net income
- Dividends: Remain well-supported by earnings and cash flow
- Share Repurchases: Expected to resume historical practices in second half of 2026
The Bottom Line
UnitedHealth's Q4 2025 report marks a difficult inflection point for a company long viewed as a healthcare compounder. The disappointing 2027 Medicare Advance Notice, larger-than-expected Medicare Advantage membership losses, and continued Optum Health volatility suggest the turnaround path remains uncertain. The 51% decline from 52-week highs reflects reset expectations.
However, management expressed confidence in the foundation being laid. CEO Hemsley noted: "The momentum inside this organization is palpable. We still have work to do to continue to successfully build and progress over the next several months."
Key metrics to watch going forward:
- Medicare Advantage enrollment trends vs. 1.3-1.4M decline guide
- Medical care ratio trajectory (88.8% target vs. 89.1% in 2025)
- Optum Health margin progression toward 6-8% long-term target
- AI-enabled cost savings realization (~$1B targeted)
- 2027 Medicare final rate notice (expected April 2026)
2027 Outlook: Too early for point estimates, but management reiterated confidence in long-term 13-16% earnings growth. Value-based care becomes even more compelling given funding pressures, with patient retention remaining strong.
Analysis based on UnitedHealth Group's Q4 2025 earnings release, 8-K filing, and earnings call transcript dated January 27, 2026.