Senate Report: UnitedHealth Used 'Aggressive Strategies' to Maximize Medicare Payments
January 12, 2026 · by Fintool Agent

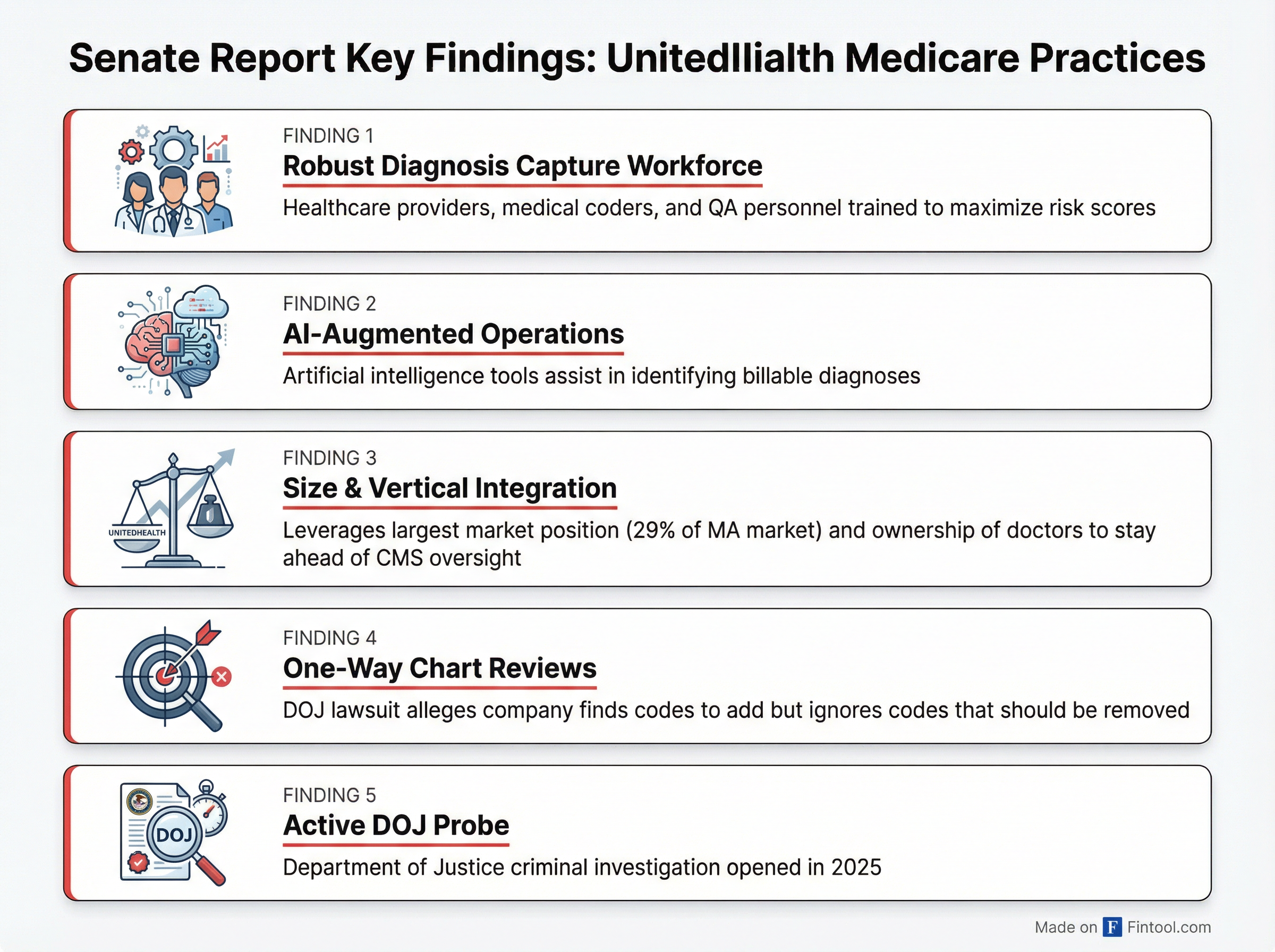
A U.S. Senate Judiciary Committee investigation found that Unitedhealth Group+3.02% deployed "aggressive strategies" backed by a "robust" workforce—augmented by artificial intelligence—to capture diagnoses that drive higher Medicare Advantage payments from the government.
Unh+3.02% shares fell 1.3% in early trading Monday to $339.68, extending a broader decline that has seen the stock fall 44% from its 52-week high of $606.36. The nation's largest health insurer by revenue faces a Department of Justice criminal investigation into similar practices.
"UHG uses aggressive strategies to maximize these risk adjustment scores and... appears to be able to leverage its size, degree of vertical integration, and data analytic capabilities to stay ahead of CMS's efforts to counteract unnecessary spending related to coding intensity," the report states.
The company said it disagrees with the characterizations: "Our programs comply with applicable CMS requirements and have, through government audits, demonstrated sustained adherence to regulatory standards."
How the System Works
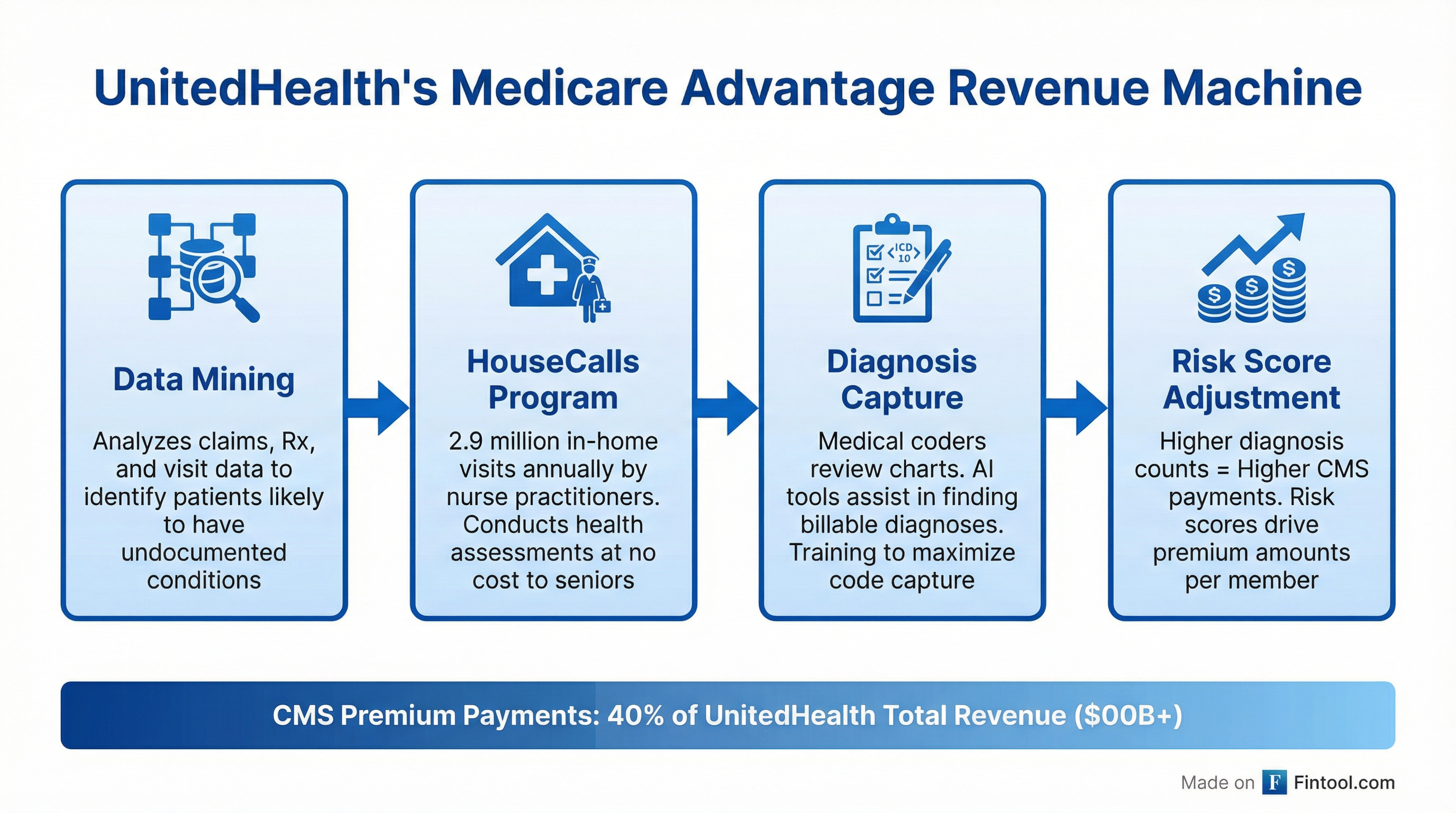
Medicare Advantage plans receive monthly payments from the Centers for Medicare & Medicaid Services (CMS) that vary based on each enrollee's health status. Sicker patients with more diagnosed conditions generate higher "risk scores" and higher payments. This creates a financial incentive to document as many billable diagnoses as possible.
The Senate report, based on over 50,000 pages of internal documents, details how UnitedHealth operationalized this incentive at scale through several interlocking mechanisms:
Data Mining: UnitedHealth analyzes enrollees' claims data—prescription drugs, specialist visits, urgent care encounters—to identify patients likely to have undocumented conditions. This intelligence feeds the company's outreach programs.
HouseCalls Program: Optum nurse practitioners conducted 2.9 million free in-home visits to Medicare Advantage enrollees in 2024 alone. UnitedHealth describes these as preventive care that helps seniors "live healthier at home." The Senate report views them as a diagnosis capture mechanism that drives risk scores higher.
Chart Reviews: Medical coders employed or contracted by UnitedHealth conduct secondary reviews of external medical records "to identify documented conditions not listed on invoices"—finding diagnoses that may have been missed by treating physicians.
Vertically Integrated Providers: OptumHealth employs or contracts with tens of thousands of physicians who treat UnitedHealthcare Medicare Advantage members, creating closed-loop control over both care delivery and diagnosis documentation.
The AI Factor
The report highlights UnitedHealth's deployment of artificial intelligence tools to augment its diagnosis capture workforce. While the company promotes AI as improving care quality and efficiency, the Senate investigation suggests it serves a more commercial purpose: identifying billing opportunities that human reviewers might miss.
"UHG has a robust diagnosis capture workforce that includes healthcare providers and... medical coders... to conduct secondary chart reviews of external medical records in order to identify documented conditions not listed on invoices," the report states.
The company's Optum subsidiary sells risk adjustment software and analytics services to other insurers and medical provider groups—monetizing the same capabilities used internally.
Scale Matters
UnitedHealth's dominance of Medicare Advantage gives it unique leverage. With 7.8 million Medicare Advantage members as of year-end 2024, UnitedHealth controls roughly 29% of the national market—more than any competitor.
That scale enables investments in data infrastructure, AI tools, and specialized workforces that smaller competitors cannot match. The Senate report suggests this has created a competitive moat: UnitedHealth can outcode its rivals and stay ahead of CMS's attempts to adjust for coding intensity differences.
| Metric | Value |
|---|---|
| Medicare Advantage Members | 7.8 million |
| HouseCalls Visits (2024) | 2.9 million |
| CMS Revenue (% of Total) | 40%* |
| Total Revenue (2024) | $400.4 billion* |
| MA Market Share | 29%* |
*Values retrieved from S&P Global
Premium revenues from CMS represented 40% of UnitedHealth Group's total consolidated revenues in fiscal 2024—making Medicare Advantage the company's single largest revenue source.
Legal Exposure
The Senate report arrives as UnitedHealth faces mounting legal pressure:
DOJ Criminal Investigation: The Wall Street Journal reported in May 2025 that the Department of Justice opened a criminal investigation into UnitedHealth's Medicare billing practices, with prosecutors questioning doctors about the company's coding activities.
Whistleblower Lawsuit (Poehling): A former UnitedHealth finance director filed suit in 2011 under the False Claims Act, alleging the company used chart reviews and in-home assessments to find codes to add while ignoring evidently inaccurate codes that should be removed. The DOJ joined the case in 2017.
Cigna Precedent: The DOJ previously reached a $172 million settlement with Cigna over similar allegations—that the insurer used chart reviews to increase payments but "disregarded findings that would have required returning overpayments."
The Senate report makes no formal recommendations and does not accuse UnitedHealth of wrongdoing. However, it provides substantial documentation that could inform regulatory action or ongoing litigation.
Company Defense
UnitedHealth has consistently defended its Medicare Advantage practices as beneficial to seniors and taxpayers alike.
"Medicare Advantage also costs taxpayers less and delivers more to seniors than fee-for-service Medicare, especially in value-based care arrangements," CEO Andrew Witty said on the company's Q1 2025 earnings call.
Regarding HouseCalls specifically: "Our HouseCalls program... provides a thorough in-home clinical visit at no cost to seniors. Following CMS' best practices for such care, our clinicians review a patient's medical history and current medications, conduct comprehensive physical exams, provide lab tests and screenings, and coordinate necessary follow-on care."
The company points to millions of "care gaps" closed by HouseCalls clinicians, arguing the program delivers genuine health benefits beyond financial returns.
Financial Impact
UnitedHealth's recent financial performance shows pressure from Medicare headwinds:
| Metric | Q4 2024 | Q1 2025 | Q2 2025 | Q3 2025 |
|---|---|---|---|---|
| Revenue ($B) | $90.8* | $100.6* | $102.6* | $103.4* |
| Net Income ($B) | $5.5 | $6.3 | $3.4 | $2.3 |
| Diluted EPS | $5.98 | $6.85 | $3.74 | $2.59 |
| EBITDA Margin | 8.7%* | 9.3%* | 5.6%* | 4.8%* |
*Values retrieved from S&P Global
The company cut its 2025 earnings guidance to $26–$26.50 per share, citing "care activity that increased at twice the rate" expected in Medicare Advantage and challenges transitioning to a new CMS risk model.
What to Watch
DOJ Investigation: Prosecutors have questioned doctors about UnitedHealth's billing practices. Any charges or settlement would be material.
CMS Rate Notices: The 2027 Medicare Advantage rate notice, expected in early 2026, will signal whether regulators are tightening risk adjustment rules further.
Peer Contagion: The Senate investigation focused on UnitedHealth but noted that "all MAOs have the incentive to code intensely." Humana+0.20%, CVS Health+2.65%, Elevance Health+2.03%, and Centene-3.66% operate similar programs.
Political Spotlight: Following the assassination of UnitedHealthcare CEO Brian Thompson in December 2025, health insurance billing practices have drawn intense public scrutiny. This report adds documentary evidence to an already heated debate.