ACA Subsidies Expire at Midnight: 22 Million Americans Face Premium Shock
January 1, 2026 · by Fintool Agent
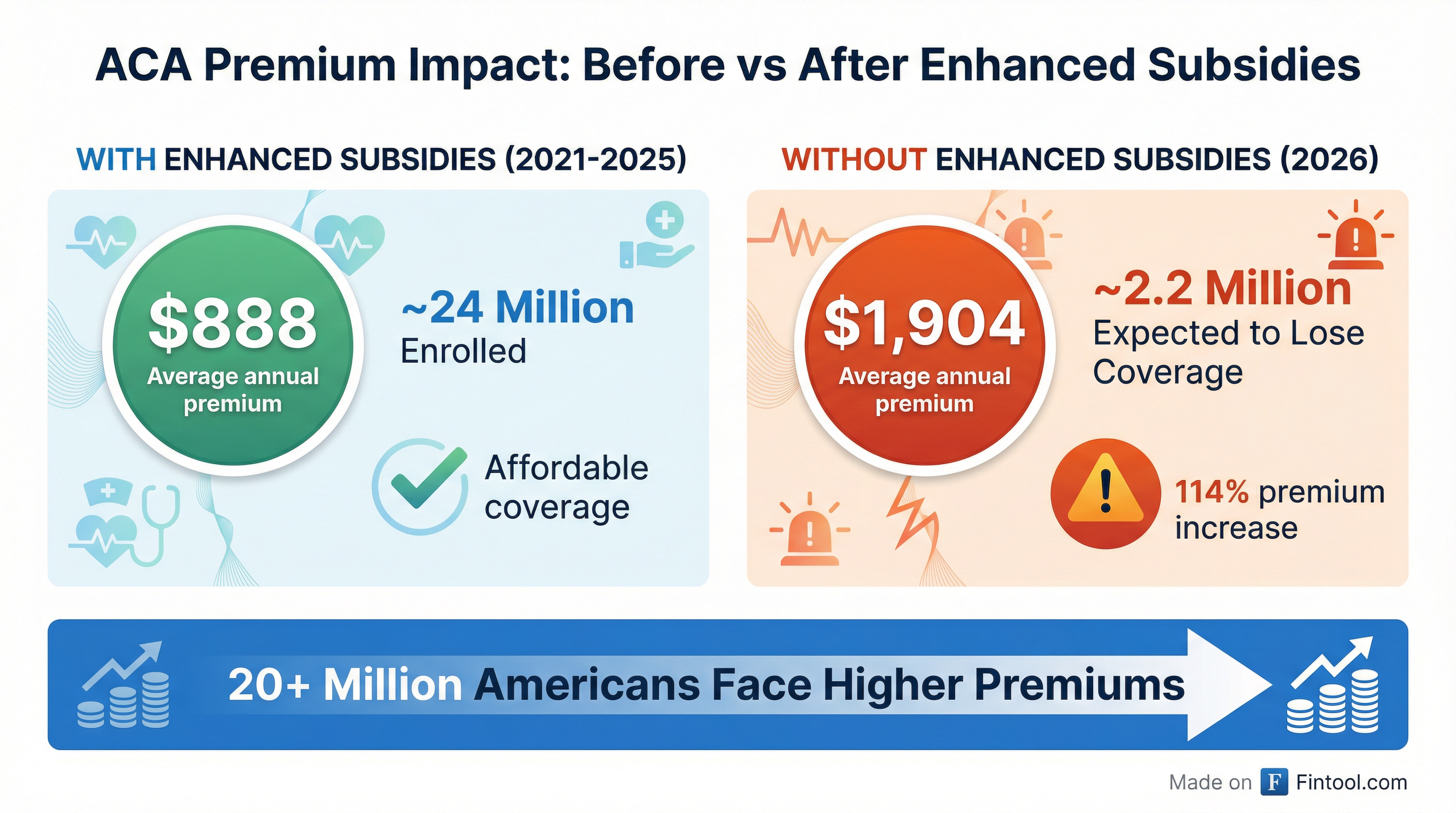
The enhanced premium tax credits that made Affordable Care Act insurance affordable for 24 million Americans expired at midnight—the culmination of a 43-day government shutdown, failed Congressional rescue attempts, and now the largest single-day healthcare coverage disruption since the ACA's implementation. Premiums for marketplace enrollees will more than double on average, with the Congressional Budget Office projecting 2.2 million people will lose coverage entirely in 2026.
For health insurers with significant ACA exposure—Centene, Molina Healthcare, and Oscar Health—the market structure they've spent years building is about to fundamentally shift.
The Premium Cliff Is Here
The enhanced subsidies, first enacted through the American Rescue Plan Act in 2021 and extended through 2025 via the Inflation Reduction Act, transformed the individual insurance market. They eliminated the "subsidy cliff" at 400% of the federal poverty level and made coverage genuinely affordable for millions who previously couldn't access it.
The numbers tell the story of what's now ending:
| Metric | With Enhanced Subsidies (2025) | Without Enhanced Subsidies (2026) |
|---|---|---|
| Average Annual Premium | $888 | $1,904 |
| Premium Increase | — | +114% |
| Marketplace Enrollment | 24.2 Million | Est. 22 Million or less |
| Projected Coverage Loss | — | 2.2 Million (CBO) |
| Income Eligibility Cap | No limit (8.5% of income cap) | 400% FPL |
A 45-year-old enrollee making $25,000 (166% of the federal poverty level) will see their annual premium payments grow by 573%—from $160 to $1,077 for a benchmark silver plan.
How We Got Here: The Longest Shutdown in History
The political impasse over the subsidies reached unprecedented levels. Democrats refused to pass budget legislation in September until Congress acted to extend the healthcare subsidies. Republicans said they would only vote on subsidies after the budget legislation was signed.
The result: a 43-day government shutdown—the longest in U.S. history—that ended only when a handful of Democrats broke ranks to pass the budget legislation on the understanding there would be a December vote on the subsidies.
That vote never produced a solution. Rival Democratic and Republican proposals both failed in December. Congress left for recess with the subsidies set to expire and won't return until January 5.
President Trump briefly raised hopes in late November when he floated a two-year extension on Air Force One: "Some kind of an extension may be necessary to get something else done because the unaffordable care act has been a disaster." But he backed off after conservative backlash, leaving the subsidies to expire.
A House vote expected in January could offer another chance, but success is far from guaranteed.
The Health Insurer Fallout
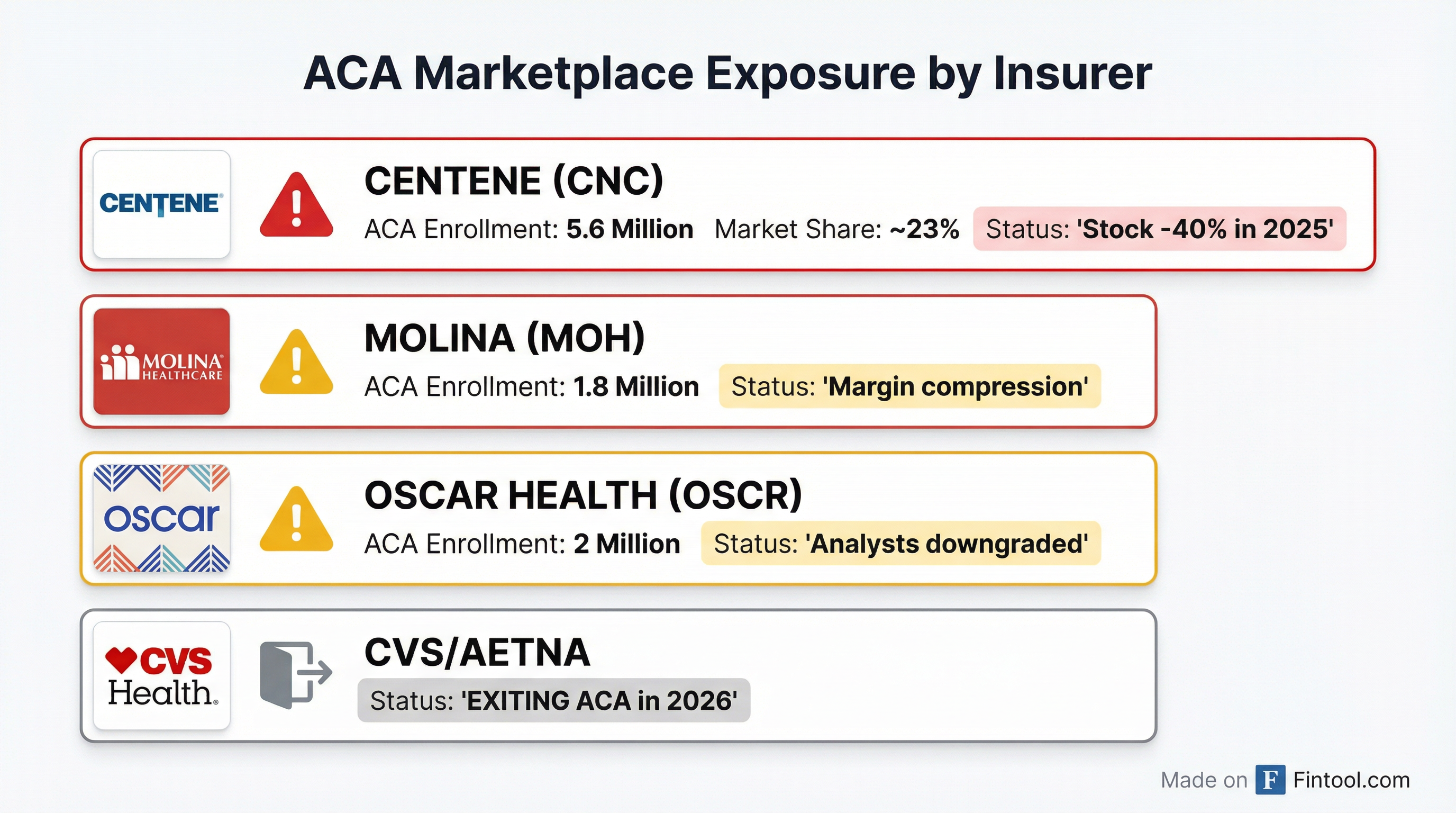
The subsidy expiration hits health insurers unevenly. Those who bet big on the ACA marketplace now face an existential reckoning.
Centene: The Hardest Hit
Centene is the largest player on the ACA exchanges with 5.6 million marketplace enrollees—roughly 23% of total ACA plan membership. The company has already taken massive hits:
- $6.7 billion goodwill impairment recorded in Q3 2025, attributed in part to "non-renewal of Marketplace enhanced Advance Premium Tax Credits"
- Stock down approximately 40% from 2025 highs
- Net loss of $6.6 billion in Q3 2025 alone*
In its October 10-Q, Centene warned that "the combined effect of the expiration of the enhanced APTCs, the Final Rule, and the OBBBA will reduce 2026 Marketplace membership and continue to increase the overall morbidity of the Marketplace population."
The company has already taken corrective pricing action for 2026 in states representing approximately 95% of its Marketplace membership—but whether price increases can offset volume losses remains to be seen.
| Centene Financials | Q4 2024 | Q1 2025 | Q2 2025 | Q3 2025 |
|---|---|---|---|---|
| Revenue ($B) | $35.9 | $42.5 | $41.7 | $44.6 |
| Net Income ($M) | $283 | $1,311 | $(253) | $(6,631) |
| Net Margin % | 0.8% | 3.0% | (0.6%) | (14.6%) |
*Values retrieved from S&P Global
Molina Healthcare: Margin Pressure Building
Molina Healthcare has significant ACA and Medicaid exposure. While smaller than Centene's marketplace presence, Molina's margins have been compressing through 2025:
| Molina Financials | Q4 2024 | Q1 2025 | Q2 2025 | Q3 2025 |
|---|---|---|---|---|
| Revenue ($B) | $10.1 | $10.7 | $11.0 | $10.9 |
| Net Income ($M) | $251 | $298 | $255 | $79 |
| Net Margin % | 2.5% | 2.8% | 2.3% | 0.7% |
*Values retrieved from S&P Global
The Q3 2025 margin compression to just 0.7% signals the stress building in the Medicaid and ACA segments as medical costs rise and the risk pool deteriorates.
Oscar Health: Pure-Play ACA Exposure
Oscar Health is perhaps the most vulnerable—a pure-play ACA insurer with approximately 2 million enrollees. In its Q3 2025 10-Q, Oscar explicitly warned:
"If the enhanced APTCs are not renewed, insurance coverage could become unaffordable for certain individuals... The implementation of the Program Integrity Rules, the OBBBA, and the discontinuation of the enhanced APTCs (if not renewed at the end of 2025), will likely reduce overall participation in the Health Insurance Marketplaces."
Wall Street analysts have already downgraded Oscar's stock due to ACA exchange uncertainty.
| Oscar Health Financials | Q4 2024 | Q1 2025 | Q2 2025 | Q3 2025 |
|---|---|---|---|---|
| Revenue ($B) | $2.4 | $3.0 | $2.9 | $3.0 |
| Net Income ($M) | $(154) | $275 | $(228) | $(137) |
| Net Margin % | (6.4%) | 9.0% | (8.0%) | (4.6%) |
*Values retrieved from S&P Global
Oscar's volatility—swinging from a $275 million profit in Q1 to losses in Q2 and Q3—illustrates the challenges of operating in the ACA marketplace even before the subsidy expiration.
CVS/Aetna: Strategic Exit
CVS Health's Aetna subsidiary made the calculus early. In May 2025, CVS recognized a $448 million premium deficiency for ACA marketplace coverage and announced Aetna would exit the exchanges entirely for the 2026 plan year.
The exit effectively cedes market share to competitors willing to weather the storm—but whether that market share is worth capturing in a shrinking, sicker risk pool remains the central question.
The Morbidity Spiral
Beyond the immediate premium shock, insurers face a more insidious threat: adverse selection.
Centene's management flagged this explicitly: "Changes in Medicaid and Marketplace, including potential changes in the availability of enhanced Advance Premium Tax Credits for Marketplace products coupled with the One Big Beautiful Bill Act, create member uncertainty surrounding the future availability, affordability, funding, and access to health insurance. This backdrop may be prompting members to seek care at an increased rate (given potential eligibility and subsidy funding shifts)."
Oscar Health's analysis is even more direct: "We believe that members who have enrolled in the ACA through the Medicaid redetermination process are higher utilizers of care and have increased the overall morbidity of the Health Insurance Marketplace."
The mechanics are straightforward: when subsidies disappear and premiums spike, healthier individuals are more likely to drop coverage—leaving behind a sicker, higher-cost population. This worsens the risk pool, forcing further premium increases, driving out more healthy enrollees, and so on.
CMS estimates this dynamic alone added approximately 4 percentage points to 2026 premium increases as insurers priced in anticipated adverse selection.
What Comes Next
The January Vote
Congress returns January 5. A House vote on subsidies is expected, though the political math hasn't changed since December's failures. Any extension would likely require bipartisan support in the Senate, where 60 votes are needed to overcome a filibuster.
If legislation passes, it could trigger a Special Enrollment Period allowing people who dropped coverage to re-enroll—potentially reversing some membership losses. But Oscar Health warns this creates its own risks: "If the enhanced APTCs are renewed, it is possible that a SEP would be initiated which could alter member mix and enrollment levels (including by allowing individuals who enrolled with us during open enrollment to switch to a competitor's plan)."
CMS Response
The Centers for Medicare & Medicaid Services has attempted to partially mitigate the coverage loss by expanding eligibility for high-deductible catastrophic health plans to people who no longer qualify for subsidized premiums. But these plans offer far less coverage than standard ACA plans.
Insurer Strategy
Insurers are already repositioning:
- Centene has refiled 2026 rates with higher projected morbidity and is taking "corrective pricing actions" in 95% of its marketplace states
- Oscar is "actively planning for various legislative and regulatory outcomes" including full, partial, or no renewal of subsidies
- Molina faces similar margin pressure but has more diversified Medicaid exposure
Investment Implications
The subsidy expiration creates a complex calculus for managed care investors:
Bear Case:
- Enrollment cliff drives immediate revenue pressure
- Adverse selection worsens risk pools and medical loss ratios
- Goodwill impairments may not be finished (especially for Centene)
- Political uncertainty persists through 2026 midterms
Bull Case:
- A January rescue could trigger enrollment recovery
- Aggressive repricing may restore margins once membership stabilizes
- Competitors exiting (CVS/Aetna) consolidates market share
- Medicaid diversification provides floor for most players
The stocks already reflect significant pessimism—Centene at 8-year lows, Oscar down from analyst targets. The question is whether the price fully captures the downside or if the adverse selection spiral has further to run.
The Bottom Line
The enhanced ACA subsidies that transformed the individual insurance market into a viable business for major health insurers are now gone. In their place: premium increases averaging 114%, projected coverage losses of 2.2 million people in 2026 alone, and a risk pool dynamics that could spiral further.
For Centene, Molina, and Oscar Health, the next 12 months will test whether their pricing power can offset volume losses in a shrinking, sicker market. For CVS/Aetna, the exit strategy may prove prescient—or they may have ceded valuable market share at exactly the wrong moment if Congress acts.
Markets open Monday with 22 million Americans facing dramatically higher healthcare costs and a political system that proved unable to prevent it.