Kaiser Permanente Pays Record $556 Million in Largest-Ever Medicare Advantage Fraud Settlement
January 15, 2026 · by Fintool Agent
Five Kaiser Permanente affiliates will pay $556 million to settle Department of Justice allegations that they systematically pressured physicians to add false diagnosis codes to patient records over nearly a decade — generating an estimated $1 billion in improper Medicare payments and producing the largest Medicare Advantage fraud settlement in U.S. history.
The settlement, announced January 14, dwarfs the previous record: Cigna's $172 million payment in 2023. Two whistleblowers who exposed the alleged scheme will receive $95 million of the recovery.
The Alleged Scheme: 500,000 Fake Diagnoses
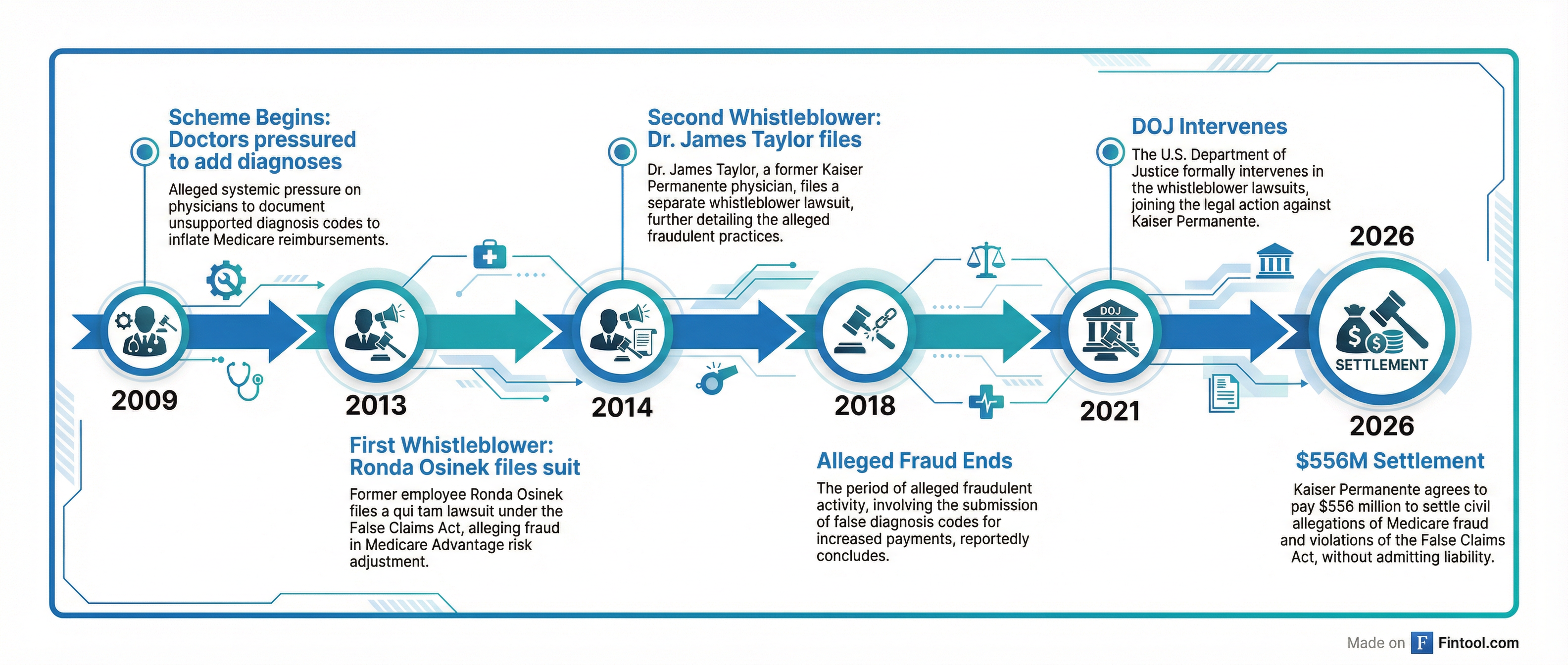
According to the DOJ complaint, Kaiser engaged in a "systematic" effort from 2009 through 2018 to inflate risk-adjusted payments from Medicare by having doctors retroactively add diagnoses to patient medical records — even when those conditions were never evaluated or treated during patient visits.
The government's investigation found:
- ~500,000 diagnoses were improperly added to patient records
- ~$1 billion in excess Medicare payments resulted from the inflated risk scores
- Kaiser tied physician bonuses to meeting diagnosis submission targets
- Internal compliance audits flagged concerns that were allegedly ignored
- The scheme spanned affiliates in California and Colorado
"Medicare Advantage is a vital program that must serve patients' needs, not corporate profits," said U.S. Attorney Craig H. Missakian for the Northern District of California. "Fraud on Medicare costs the public billions annually, so when a health plan knowingly submits false information to obtain higher payments, everyone — from beneficiaries to taxpayers — loses."
How Medicare Advantage "Risk Adjustment" Works
Medicare Advantage plans receive fixed monthly payments from the Centers for Medicare & Medicaid Services (CMS) for each enrolled beneficiary. CMS adjusts these payments based on how sick patients appear to be — paying more for members with serious conditions and less for healthier ones.
This creates an incentive structure that prosecutors say Kaiser exploited. By adding diagnosis codes for conditions patients didn't actually have, Kaiser allegedly made its member population appear sicker than it was, triggering higher payments.
The practice is known in the industry as "upcoding" — and it has drawn increased regulatory scrutiny as Medicare Advantage has exploded in popularity, now covering over 34 million Americans, more than half of all Medicare-eligible individuals.
The Whistleblowers: A Decade-Long Fight
The settlement resolves two qui tam lawsuits filed under the False Claims Act by former Kaiser employees:
Ronda Osinek, a medical coder who filed her complaint in August 2013, alleged Kaiser systematically inflated claims by having doctors amend medical files — often months after patient visits — to add diagnoses that were never treated or didn't exist.
Dr. James M. Taylor, a physician who oversaw risk adjustment programs and coding governance at Kaiser, filed his lawsuit in October 2014. His attorneys described the case as a "long, hard-fought" battle.
"It's important to send a signal to the industry, and this number hopefully does that," said Max Voldman, an attorney representing Dr. Taylor.
The DOJ intervened in both cases in July 2021, consolidating them and filing detailed allegations against Kaiser. Under the False Claims Act's qui tam provisions, whistleblowers can sue on behalf of the government and share in any recovery. Osinek and Taylor will split $95 million.
Record Settlement in Context
The $556 million payment is more than triple the previous largest Medicare Advantage fraud settlement.
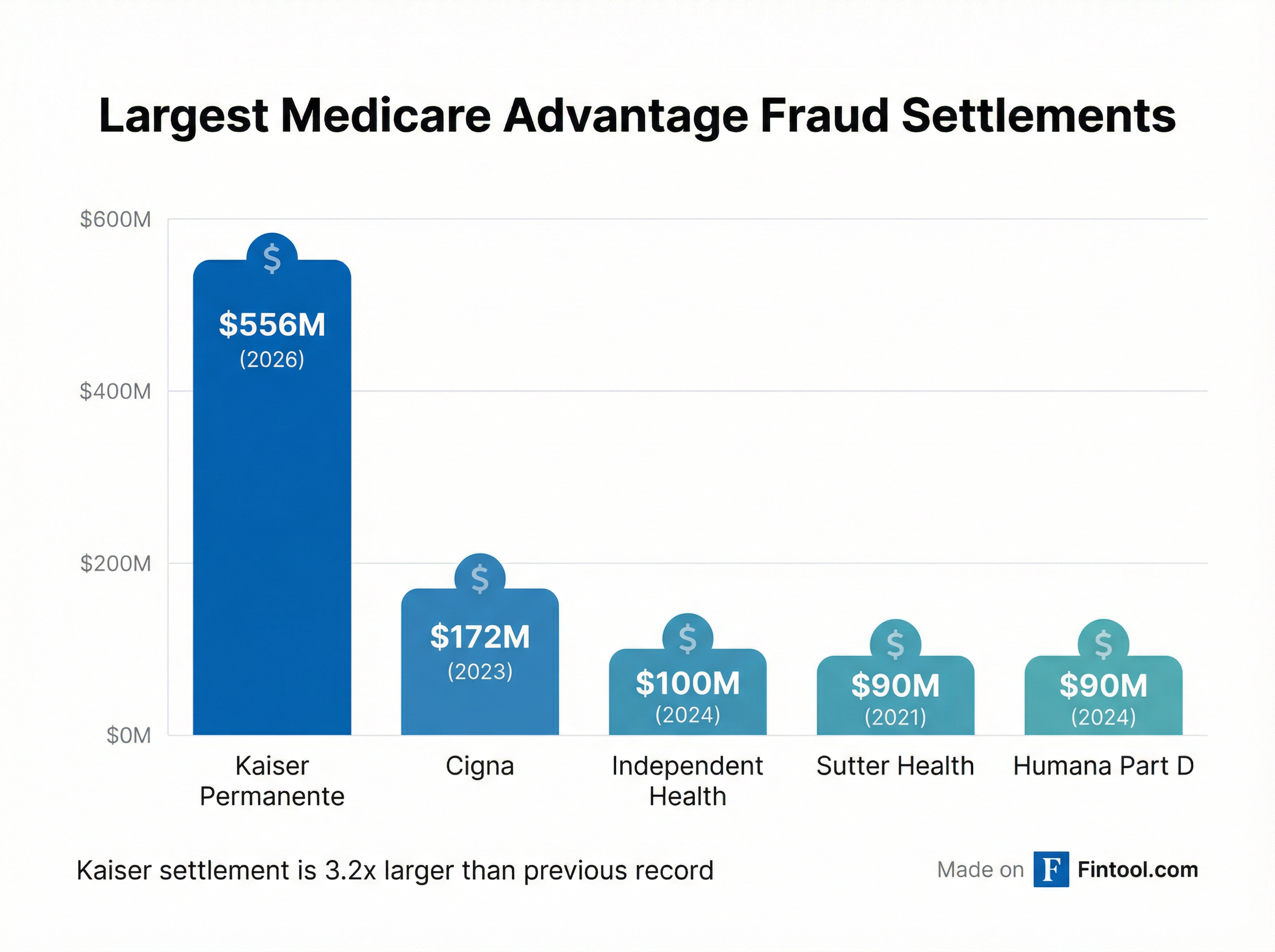
| Settlement | Year | Amount |
|---|---|---|
| Kaiser Permanente | 2026 | $556M |
| Cigna | 2023 | $172M |
| Independent Health | 2024 | $100M |
| Sutter Health | 2021 | $90M |
| Humana (Part D) | 2024 | $90M |
The settlement comes on the heels of a Senate Judiciary Committee report this month accusing UnitedHealth Group of "gaming" the Medicare Advantage payment system. Senator Chuck Grassley (R-Iowa), who chairs the committee, said his investigation reviewed over 50,000 pages of internal company documents.
"Bloated federal spending to UnitedHealth Group is not only hurting the Medicare Advantage program, it's harming the American taxpayer," Grassley said.
The DOJ also has pending False Claims Act litigation against UnitedHealth over similar risk adjustment allegations, as well as a separate case accusing Aetna, Anthem, and Humana of paying hundreds of millions in illegal kickbacks to insurance brokers.
Kaiser's Response: "Industrywide Challenges"
Kaiser did not admit wrongdoing in the settlement. In a statement, the company said it "chose to settle to avoid the delay, uncertainty, and cost of prolonged litigation."
The health system argued the case reflected "industrywide challenges in applying these requirements" for Medicare Advantage risk adjustment, noting that "multiple major health plans have faced similar government scrutiny."
"The Kaiser Permanente case was not about the quality of care our members received," the company said. "It involved a dispute about how to interpret the Medicare risk adjustment program's documentation requirements."
The settling affiliates include:
- Kaiser Foundation Health Plan Inc.
- Kaiser Foundation Health Plan of Colorado
- The Permanente Medical Group Inc.
- Southern California Permanente Medical Group
- Colorado Permanente Medical Group P.C.
Kaiser is the sixth-largest Medicare Advantage provider in the country, covering about 6% of MA members, according to Kaiser Family Foundation data. The Oakland, California-based healthcare consortium operates dozens of hospitals and serves millions of members.
What This Means for the Industry
The record settlement signals that the Trump administration is continuing aggressive enforcement against Medicare Advantage billing practices — a priority that spans multiple administrations.
Medicare Advantage is a $450 billion annual program that has grown rapidly as insurers market the plans' additional benefits compared to traditional Medicare. But that growth has come with mounting concerns about systematic overbilling.
A 2022 New York Times investigation found that eight of the ten largest Medicare Advantage providers had faced fraud allegations, whistleblower lawsuits, or inspector general findings of overbilling. The government's auditors have estimated billions in annual overpayments due to improper diagnosis coding.
For insurers with significant Medicare Advantage exposure — including Unitedhealth Group+3.02%, Humana+0.20%, CVS Health+2.65%, and Elevance Health+2.03% — the Kaiser settlement reinforces that risk adjustment practices remain under intense regulatory scrutiny.
What to Watch
-
Pending UnitedHealth litigation: The DOJ has intervened in at least two False Claims Act cases against UnitedHealth over similar risk adjustment allegations. Given the scale of UnitedHealth's MA business — 27% market share — any settlement could dwarf even Kaiser's.
-
Regulatory changes: CMS has proposed tightening risk adjustment audit rules, which could increase recovery of overpayments and create additional compliance costs for MA plans.
-
Senate oversight: Senator Grassley's report suggests continued congressional scrutiny of Medicare Advantage billing, which could lead to legislative action on risk adjustment reform.
-
Whistleblower pipeline: The Kaiser case took over a decade from initial filing to settlement. Multiple similar cases remain pending against other insurers, suggesting more large settlements could emerge in coming years.
Related Companies: Unitedhealth Group+3.02% · Humana+0.20% · CVS Health+2.65% · Elevance Health+2.03% · Cigna Group+2.64% · Centene-3.66%